Preventing Suicide: The Importance of Keeping an Open Conversation about Mental Health
By Dr. Scott Reisinger
Every September, our nation observes Suicide Prevention Awareness Month. While this stigmatized topic may be difficult to discuss, and even considered taboo by some, it’s critical to the public health of our communities that we promote an open dialogue about mental and behavioral health.
Suicide is the second leading cause of death for people between the ages of ten and thirty-four, and the overall rate of suicide has increased 35% over the last tenty-three years. Taking time to listen, offer help and eliminate stigmas around seeking mental health support can sometimes make all the difference in helping someone experiencing suicidal thoughts.
There is no special training needed to start a conversation about mental health and suicide prevention. Keeping lines of communication open with your family and friends can make it easier for them to discuss any difficult feelings they may be experiencing and recognize they’re not alone.
We have all felt anxious, sad, depressed, grieved, angry or even lost at some time in our lives. However, sometimes these feelings can feel make a person feel like they are on an island. By offering a listening ear and platform for an understanding, supportive conversation, you can sometimes help soften those feelings of isolation.
One way to start the conversation about mental health and suicide is to pick an environment where your loved one will feel most comfortable. From there, you may share that you have noticed they don’t seem like their usual self, and you may even describe the changes you’ve noticed in their mood or behavior.
During these difficult conversations, comments such as “what happened next” or simply stating “I understand” can reinforce that you are actively listening to what they are saying. Using phrases like, “what can we do to make things better?” and “I’m here for you,” as opposed to offering advice, can also be effective. Let your loved one know that you understand how hard it is to talk about their feelings and reassure them that conversations like these are a positive step forward.
Mental Health Stigmas
These conversations are also essential to breaking down the stigmas that plague mental health and keep people from seeking help. While some can manage feelings of anxiety or depression and recover on their own, others may require additional assistance, using tools such as therapy or medications. Unfortunately, our society has stigmatized seeking help for mental illness when there’s no reason why it should be viewed any differently than a medical illness.
It is important to remember that your loved one may feel ashamed to ask for help, or may not know where to start. Any significant stressor, particularly one that is ongoing, will tax a person’s resources and resiliency, especially if they are not properly caring for themselves.
This can exacerbate anxiety and depression in anyone. Understanding the underlying reason behind any harmful thoughts and feelings is essential to addressing them and developing healthy coping skills with the help of professionals.
Where to Seek Help
If you or a loved one are experiencing harmful thoughts and you don’t know where to seek help, contact a behavioral health consultants or therapist in your area. They can assess if the individual will benefit from brief, solution-focused, skills-based intervention to address a multitude of concerns, in addition to anxiety and depression, or if the individual would be better served by referral to a provider in the community for more “traditional” counseling or psychotherapy.
The research is clear. Asking about and discussing depression and suicide does not increase risk of an individual attempting suicide. In fact, it may open the door for the person to express how they are feeling and ask for the help they need. In fact, it reduces the risk overall.
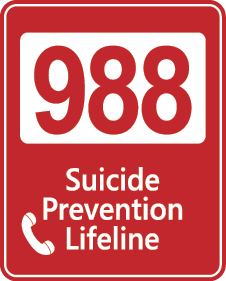
If you or a loved one needs someone to talk to, you can call the National Suicide Prevention Lifeline 24/7, at 1-800-273-8255 (TALK) or you can dial 988. These calls offer free and confidential support to those in suicidal crisis or emotional distress. You can also reach to your health care provider to learn more about additional resources and help available to you and your loved ones. This month, and every month, let us continue to have open and honest conversations about mental and behavioral health.
*Scott E Reisinger, PsyD, is a National Register credentialed Health Service Psychologist for Mercy Health. He has trained as a generalist, specialized in health psychology and is a graduate of the Georgia School of Professional Psychology.
Every September, our nation observes Suicide Prevention Awareness Month. While this stigmatized topic may be difficult to discuss, and even considered taboo by some, it’s critical to the public health of our communities that we promote an open dialogue about mental and behavioral health.
Suicide is the second leading cause of death for people between the ages of ten and thirty-four, and the overall rate of suicide has increased 35% over the last tenty-three years. Taking time to listen, offer help and eliminate stigmas around seeking mental health support can sometimes make all the difference in helping someone experiencing suicidal thoughts.
There is no special training needed to start a conversation about mental health and suicide prevention. Keeping lines of communication open with your family and friends can make it easier for them to discuss any difficult feelings they may be experiencing and recognize they’re not alone.
We have all felt anxious, sad, depressed, grieved, angry or even lost at some time in our lives. However, sometimes these feelings can feel make a person feel like they are on an island. By offering a listening ear and platform for an understanding, supportive conversation, you can sometimes help soften those feelings of isolation.
One way to start the conversation about mental health and suicide is to pick an environment where your loved one will feel most comfortable. From there, you may share that you have noticed they don’t seem like their usual self, and you may even describe the changes you’ve noticed in their mood or behavior.
During these difficult conversations, comments such as “what happened next” or simply stating “I understand” can reinforce that you are actively listening to what they are saying. Using phrases like, “what can we do to make things better?” and “I’m here for you,” as opposed to offering advice, can also be effective. Let your loved one know that you understand how hard it is to talk about their feelings and reassure them that conversations like these are a positive step forward.
Mental Health Stigmas
These conversations are also essential to breaking down the stigmas that plague mental health and keep people from seeking help. While some can manage feelings of anxiety or depression and recover on their own, others may require additional assistance, using tools such as therapy or medications. Unfortunately, our society has stigmatized seeking help for mental illness when there’s no reason why it should be viewed any differently than a medical illness.
It is important to remember that your loved one may feel ashamed to ask for help, or may not know where to start. Any significant stressor, particularly one that is ongoing, will tax a person’s resources and resiliency, especially if they are not properly caring for themselves.
This can exacerbate anxiety and depression in anyone. Understanding the underlying reason behind any harmful thoughts and feelings is essential to addressing them and developing healthy coping skills with the help of professionals.
Where to Seek Help
 If you or a loved one are experiencing harmful thoughts and you don’t know where to seek help, contact a behavioral health consultants or therapist in your area. They can assess if the individual will benefit from brief, solution-focused, skills-based intervention to address a multitude of concerns, in addition to anxiety and depression, or if the individual would be better served by referral to a provider in the community for more “traditional” counseling or psychotherapy.
If you or a loved one are experiencing harmful thoughts and you don’t know where to seek help, contact a behavioral health consultants or therapist in your area. They can assess if the individual will benefit from brief, solution-focused, skills-based intervention to address a multitude of concerns, in addition to anxiety and depression, or if the individual would be better served by referral to a provider in the community for more “traditional” counseling or psychotherapy.
The research is clear. Asking about and discussing depression and suicide does not increase risk of an individual attempting suicide. In fact, it may open the door for the person to express how they are feeling and ask for the help they need. In fact, it reduces the risk overall.
If you or a loved one needs someone to talk to, you can call the National Suicide Prevention Lifeline 24/7, at 1-800-273-8255 (TALK) or you can dial 988. These calls offer free and confidential support to those in suicidal crisis or emotional distress. You can also reach to your health care provider to learn more about additional resources and help available to you and your loved ones. This month, and every month, let us continue to have open and honest conversations about mental and behavioral health.
*Scott E Reisinger, PsyD, is a National Register credentialed Health Service Psychologist for Mercy Health. He has trained as a generalist, specialized in health psychology and is a graduate of the Georgia School of Professional Psychology.

Monthly newsmagazine serving people of Irish descent from Cleveland to Clearwater. We cover the movers, shakers & music makers each and every month.
Since our 2006 inception, iIrish has donated more than $376,000 to local and national charities.
GET UPDATES ON THE SERIOUS & THE SHENANIGANS!